Your period is like your monthly report card- it’s your body’s way of telling you if something is out of whack. So what does it mean if your period is missing?? There could be many reasons for this, a common condition is Hypothalamic Amenorrhea (HA).
Hypothalamus = gland in brain that send message for ovulation
Amenorrhea = absent periods
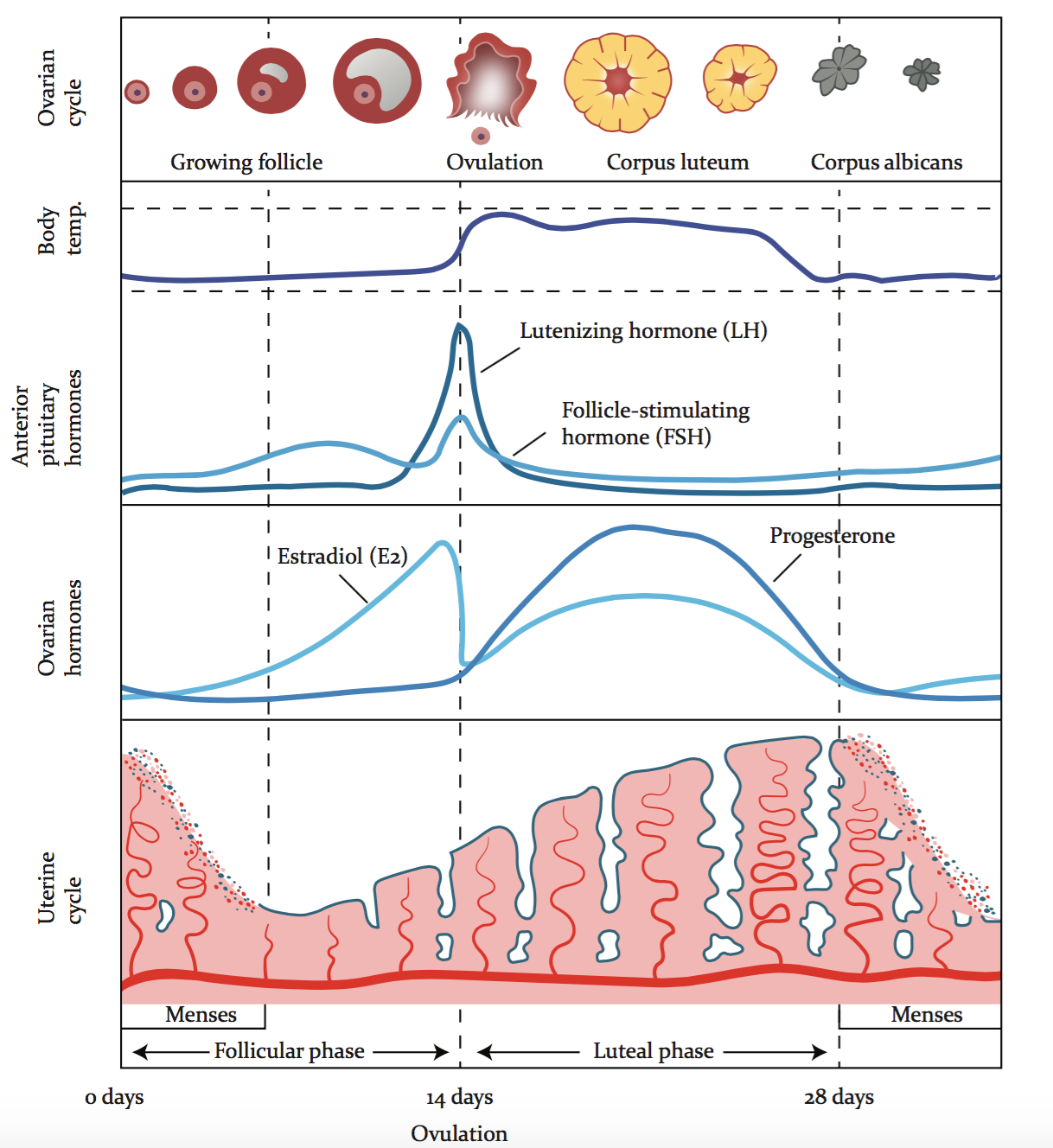
Having regular healthy periods are a sign of good health and healthy ovulation. Without ovulation you cannot make a baby, nor can you make all the beautiful hormones that benefit our mood, hair, metabolism, skin, bones and heart health. When your hormones are in balance and harmony, you can have, and you should have, healthy, comfortable and pain-free periods.
Hypothalamic Amenorrhea (HA) is a condition where a woman's menstrual period is missing for more than six months.
For a diagnosis, all other medical conditions that could possibly explain the lack of period must be ruled out - it is kind of like a process of elimination. If you have recently stopped taking the oral contraceptive pill, this could be why your period is missing - this is different to HA.
Remember, the pill shuts down ovulation. It is common to take a few months, post-pill, before your brain relearns how to communicate with the ovaries again, in order to ovulate and have a period.
HA is usually a sign that the body is going into survival mode - The body doesn’t feel safe and doesn’t feel capable of ovulating and bringing new life into the world. The main purpose of the reproductive cycle is to reproduce, right? The reproductive organs differ from other organs, like our heart, lungs and brain that are crucial for our survival. Although the reproductive system is super important, it is not essential to survive.
What causes HA?
HA is usually caused by under eating, high stress, and overexercising. When we are not nourishing our bodies with enough food, the body is very clever, and preserves those calories and nutrients for more crucial organs. If we are putting ourselves under too much pressure and stress, the brain is thinking… “Now is not the right time to make a baby, the body doesn’t have the nutrients or mental capacity to support a growing baby” So what does it do? It shuts down ovulation to prevent pregnancy and will present with a missing period.
The body cannot differentiate between “good stress” and “bad stress”. It is all “stress”. When we exercise at a high intensity it is putting the body under stress. This is not always a bad thing… However, even if you are not “over exercising”, high intensity exercise can still be a contributing stressor in HA cases.
You can exercise - as long as you eat enough!
What are the symptoms of Hypothalamic Amenorrhea?
The most obvious symptom of HA is a missing period. But there are other symptoms that are less obvious such as:
low libido
increased bone loss
mood changes
low energy
thinned uterine lining
most of these are due to low oestrogen
Some women with HA have polycystic ovaries, this does not always mean they have the syndrome PCOS.
It is common for women to be misdiagnosed with PCOS when they have HA because of many similarities between the symptoms. It is important to understand why your period is missing, to get the right diagnosis, to direct the right treatment.
HA treatment is generally to eat more food. Whereas, PCOS treatment can often involve managing testosterone and insulin levels. You can see why it is pretty important to get the right treatment? Read more on the different types of PCOS here.
Testing:
If you lost your period to under eating which has caused HA, you likely will have one or more of the following signs:
no withdrawal bleed from the pill
low fasting insulin (less than 4 mIU/L or 25 pmol/L)
low ratio of luteinising hormone (LH) compared to follicle-stimulating hormone (FSH)
So: Are you eating enough to get a period?
If you were my patient, I would ask you “Do you feel like you are getting enough to eat? For example, yesterday - did you feel satisfied with your food?”
You need to be eating a combination of fats, proteins AND carbs to have a balanced intake to support your hormones.
Remember:
Going on hormonal birth control is not an effective treatment for HA because a bleed on the pill is not a real period.
If you are still confused as to why your period is missing, it is important to get the right support to help you to receive the correct diagnosis and treatment.
If you’re scared by the idea of eating more, please reach out for help to discuss whether you may have an eating disorder. Eating disorders are common and are nothing to be ashamed of - approaching your eating with self-love and self-forgiveness, and know you’re not alone.
Please reach out to me for more help to get your menstrual cycle sorted.
Book a free assessment here